Warts and Sarcoid Tumors in Horses
Warts and sarcoid lumps are common skin growths in horses and may be hard to differentiate because they can be similar in appearance.
Andrew D. Smith, DVM, PhD, DACVS-LA, Clinical Assistant Professor of the Department of Large Animal Clinical Sciences at the University of Florida College of Veterinary Medicine, says most warts are seen on young horses, usually around the nose and muzzle, and these are generally a temporary problem. “Here at our hospital we only see the challenging cases from veterinarians who refer them to us. Most of the time, the warts that occur in younger animals are not a problem,” he says.
“Most of these are associated with equine papilloma virus 1, but they can have several forms or subcategories. We also see aural plaques, which are warts in the ears, which also don’t tend to regress.
“Here at our hospital, we rarely see the most common ones unless that horse is coming in for some other reason like lameness, colic or some other problem. If the horse also happens to have warts, we show them to our students and tell them this is what warts look like and explain that at this point we tend to just leave them alone. Within a couple of months those warts will regress, and the horse will have a lifelong immunity and never get warts again.”
These warts are contagious in that they can be transmitted between horses or spread by flies or some sort of fomite that takes the virus from one horse to another, such as grooming tools or tack used on multiple horses. “Usually if a farm has one young horse with warts, there will soon be many with warts,” says Smith. “The whole group of yearlings may have warts,”
Those warts usually don’t become a problem unless they become so large or numerous around the mouth and muzzle that they interfere with eating, breathing, or use of a bit. “We usually don’t have to treat this type of warts,” he says.
Warts on the penis are more problematic. “If a horse is referred to me for treatment, it is usually because the warts involve the entire glans penis,” he explains. “We usually have to remove those by freezing them or doing a partial phallectomy (removal of part of the penis). This may be a little drastic, but horses with partial phallectomies do very well. Treating them any other way doesn’t get to the root of the problem to get rid of them.
“If these warts are small and localized, we can freeze them or remove them with a laser. If we do a partial phallectomy, the horse would not be useable for breeding so we do those only in geldings. A partial phallectomy doesn’t work very well in stallions. If they get an erection during the first couple months while those tissues are still healing, this increases the risk for surgical site dehiscence (rupturing) and breaking the sutures.
“Hypothetically, you might be able to do this surgery on a stallion and still be able to collect him if you were able to keep him from getting an erection until the surgical site was fully healed, but I don’t know of anyone who has done that. Usually, you’d find the warts earlier in a breeding stallion and be able to remove them before they become so large that a partial phallectomy would be necessary, because someone is looking at the penis more often than just twice a year.”
A gelding is more likely to end up with larger growths before they are discovered. In early stages, the penile warts could be removed with a laser or by freezing, and the stallion would be able to continue breeding. Usually those warts start out with just one or two, but by the time you see this in a gelding there might be 50, or it may have progressed to squamous cell carcinoma. A person might pull the penis out to clean it and wonder what the huge mass is. “This is usually when I see the horse,” says Smith. “They don’t send me the ones that have just one or two small warts. There are some things you can do with those early on, but those are the easy ones that I rarely get to see.”
There is also a congenital form of warts where the foal is born with them. “Those generally don’t regress. They may be located on the forehead, nostrils, lower lip, and sometimes around the thorax or hind legs. These need to be removed,” he says.
The only warts that actually regress are in young horses that are normal at birth and then encounter the papilloma virus in their first year or two of life. Those warts usually appear around the face and muzzle, grow larger for a while, and then regress as the horse builds up an immunity to them. “We tell horse owners to just watch them to see if they regress. It’s usually the warts in older horses that we end up having to remove surgically.”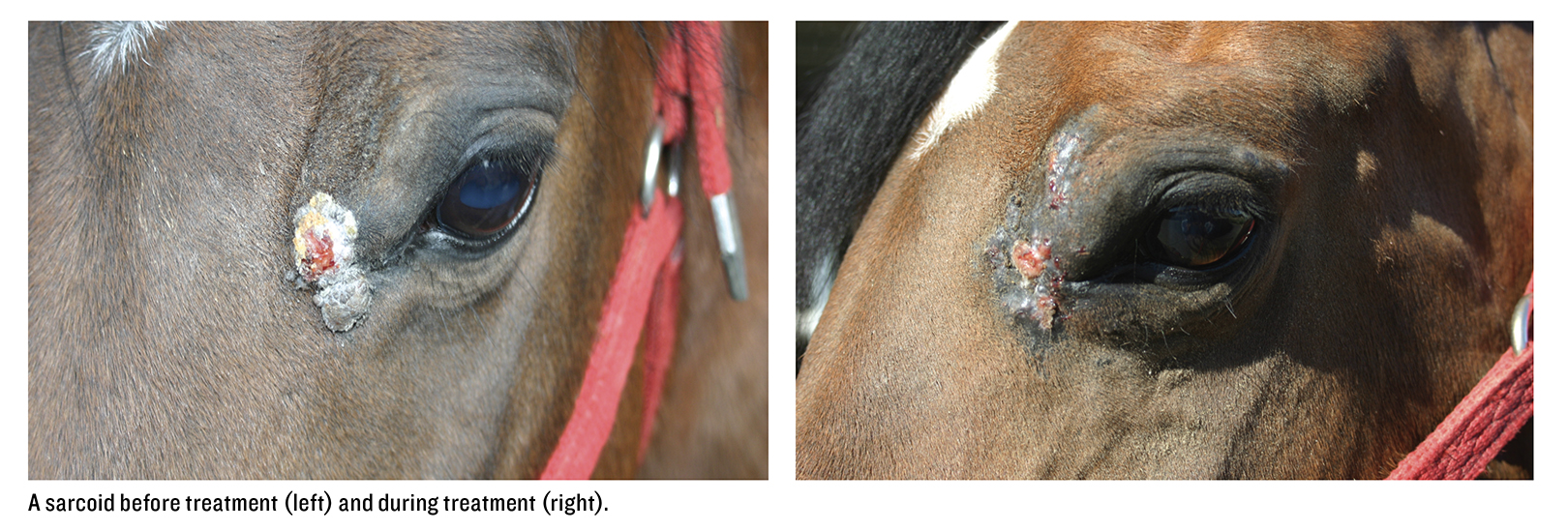
Sarcoid
Sarcoids are skin tumors that sometimes look like warts or proud flesh, or occasionally, look like ringworm. There are several types of sarcoid. Some are slow-growing and some are more aggressive, but most of them do not regress. If you biopsy the lesion, the sarcoid often gets worse.
Smith generally sees the severe cases because he works at a referral hospital. “I rarely get to see a dormant sarcoid or one that hasn’t been previously treated. We may see one in a horse that is coming in for some other reason like colic, an orthopedic issue or some other problem. We might notice the sarcoid and mention it to the client, but generally don’t do much about it because the horse is here for another reason and the owners don’t want to do anything about it,” he says.
There are six types of sarcoid: occult, verrucous, nodular, fibroblastic, mixed forms and malignant. Sometimes these are very distinctive, but often there’s a blurring of the margins. The hairless ones might have one little wart-like region, but there can be mixes of each. “We rarely see the classic forms by themselves,” says Smith.
The occult form is basically flat, hairless and often small and circular. “They are sometimes more extensive, but usually appear around the mouth or eyes, on the neck or medial aspects of the limbs, or on hairless regions of the body,” he says. “Sometimes they are hardly noticed. You may just see a little bit of pigment change in the skin. These are the ones I rarely get to see unless the horse comes in for some other reason.
“I was taught to leave occult sarcoids alone as some of these will regress on their own, but the literature has now gone back and forth regarding this. If they do regress, however, those horses are generally free of sarcoid for the rest of their lives. The body recognizes them, fights them off, and those horses develop an immunity.
“If they are extensive or in an area that’s not susceptible to trauma, I usually leave those alone and have the owner just watch them to see if they get bigger. In an area that is likely to suffer trauma, like the girth region, we try to remove them. Most of the ones we see start out as small and quiescent but may be subject to some sort of trauma. If they are on the face or girth or along the horse’s side, the tack rubs them.”
Any rubbing or trauma may irritate them and cause them to grow. “Trauma is usually what results in progression from less aggressive forms,” he says.
Verrucous sarcoid growths are wart-like, grey and scaly, but extend deeper into the tissues than the occult sarcoid. “Sometimes they have a circular hairless patch around them that might look a little bit like ringworm, but because they are warty there may be multiple different types of lesions together. Both the occult and the verrucous sarcoid are usually slow-growing and not very aggressive, but are susceptible to trauma that may stimulate them to grow. These are the ones that are usually mistaken for warts. They both have that typical hyperplastic warty appearance,” says Smith.
Nodular sarcoid can be type A or type B. “Type A has no cutaneous involvement, while type B usually has cutaneous involvement. They are both nodular in shape and just look like nodules underneath the skin, usually with the hair still covering them. They just look like a firm lump under the skin and you don’t really see anything that would make you think it’s a sarcoid. They generally form in specific locations, such as around the eye or the medial aspect of the legs,” he says.
Fibroblastic sarcoids are basically nodular but hairless. “They look like masses with ulcerated margins. They can either be pedunculated masses (on a stem) or have a broad base. They may be ulcerated or look like granulomatous lesions. As such, they might be mistaken for any number of things, such as exuberant granulation tissue (proud flesh), squamous cell carcinoma, cutaneous habronemiasis, pythiosis, etc. These growths can be very large and broad-based,” says Smith.
Mixed forms are basically a mix of verrucous, nodular and fibroblastic. “Some portions may have a specific appearance, whereas others go into the other types,” he says.
Malignant sarcoid is fairly rare. “Usually these are just a large, mixed form that is locally aggressive and continues to grow. I’ve seen some that have taken over an area and are rapidly growing, such as all the way down a leg or whole portions of the face. There is no real treatment for those. Trying to keep these horses alive could be grounds for animal cruelty, since these growths are very pruritic (itchy) and the horse will be miserable. The other types tend to be painless,” he says.
Treatments For Sarcoid
It’s usually best to leave most sarcoids alone, because if they are biopsied or removed, they often grow back in larger, more aggressive form. Surgery is one of the more common treatments, but the veterinarian may use cryotherapy first, which involves freezing the tissue to debulk it, which is what would usually be done in a human.
“We usually get to see the ones that people have unsuccessfully tried to treat and that haven’t responded to medical therapy, such as Xxterra, 5-Fluorouracil, Imiquimod, BCG, etc. I am not saying that these treatments haven’t been used effectively to treat some sarcoids. I only see the ones that recurred after these treatments have failed,” says Smith.
“I tell people that you shouldn’t just poke the bear. You either need to shoot the bear or leave the bear alone. Don’t poke it to see what happens! If the bear is asleep, leave it alone,” he says. Surgery is probably one of the more common treatments for sarcoids that have to be removed for some reason, but the goal is to remove all of it.
“The veterinarian would generally make a decision regarding treatment based on the size and form of the growth. The fibroblastic sarcoids are more likely to be treated surgically. Location makes a difference also, since we can’t really excise the tissue around the eyes or on the eyelids,” he says.
For sarcoid lesions around the eyes, a common treatment is an injection of BCG (Bacillus Calmette-Guerin), which is an immune stimulant. “This produces a lot of inflammation and makes the area very angry, and hopefully stimulates an immune response so the body will fight the tumor,” says Smith.
If this works, the sarcoid becomes ulcerated and then falls off. Because of the swelling and inflammation, the horse may be put on drugs to help control that secondary inflammation. “One risk when using BCG is the possibility of side effects, which could include anaphylactic reactions,” he says.
“A lot of the sarcoids around the eyes involve the eyelid, which means you can’t surgically remove them, so we use some kind of localized treatment like BCG or cisplatin which is a type of chemotherapy.”
The drug that’s been reported to have the most success is called platinol or cisp-platinum in oil, but requires special handling so not all veterinarians use it. The person administering it needs to wear gloves, protective clothing and use special disposal. It also requires repeat injections of the area using a special needle system. According to some reports, this treatment can be 100% effective. This drug should not be used in breeding animals, however, or any horses with impaired kidney function.
Radiation therapy is used on some sarcoid lesions, but only a few hospitals offer this form of treatment. “Although this is an effective treatment option, the drawback is that the horse usually needs to be anesthetized for each treatment so owners generally shy away from it.” Chemotherapy has also been found useful in treating equine sarcoid.
“Most of what I do is surgical removal followed up by chemotherapy, since I am generally dealing with growths that other people have tried to put BCG on, or 5FU (Fluorouracil, which is a medication used to treat cancer), or Imiquimod cream (which is used to treat certain types of scaly growths on the skin or to treat superficial basal cell carcinoma), or some other topical treatments that merely poked the bear. If people are using those sorts of things, however, it’s probably because they’ve had some success doing it with some cases. If you read the literature, this seems to be true,” says Smith.
The size of the lesion makes a difference in how it is treated. “Probably no treatment would work very well for a really large fibroblastic mass. Most of what we know about sarcoids goes back to their cause (bovine papilloma virus) and treatment may not be as effective as we’d like it to be,” he says.
The virus enters the skin via an opening in the skin, such as trauma or fly bites. “The virus may lie dormant for many years in the skin. Studies have shown that biopsies from normal horses (30 to 40%) are positive for the virus. More than 90% of sarcoids sampled contain bovine papilloma virus, so we know it’s a big player.
“Sarcoids in general are not very well circumscribed masses. The sarcoid has little fingers that go in all directions. They are similar to the root system of a tree in that some of it is beneath the surface. The tumor and/or virus infiltrates a wide area beneath the surface of the skin. If you chop a tree off at the base, you haven’t removed the root system underneath. The reason there’s a lot of treatment failure is that many people simply chop off what they can see. They don’t treat the root system underneath, and the sarcoid may regrow.
“Unlike melanomas, which usually are very well circumscribed (you can tell the limits of these growths and can remove them), with sarcoids we very rarely get all the margins. If you don’t treat the base, they will just recur. One reason they recur is that the papilloma virus is there, surrounding the sarcoid. Since you merely excised it and created inflammation, the inflammation stimulates more growth. In horses that have the virus in their skin, we think that all they need is a traumatizing event to get it going,” he says.
The virus may have entered the horse’s skin years earlier - even 10 to 15 years before - and then the horse starts getting sarcoids. “This is what we think happens with most of the cases that occur on the limbs. They are often getting bumped, scraped or nicked, which might stimulate the virus to create the growth. So when you go in there surgically and do that, you cut down the tree but forgot to remove the root system and it regrows.
“That’s why when people ask if I want to biopsy a growth to see if it’s a sarcoid, I tell them absolutely not. Either I am going to remove all of it and treat the base to remove the roots as well, or I am going to just watch it to see if it grows. If it starts to enlarge, that’s when you want to remove all of it. If you traumatize it, it just turns it into a more aggressive form.
“Another reason some sarcoids recur after treatment is that most practitioners don’t have use of a laser or other tools that can excise tumors without spreading them by inoculating the tumor bed. When you cut the tissue with a blade (unless you can get huge margins around it, which rarely happens for me because I am usually doing the very large sarcoids), you inoculate the surrounding tissue with the virus. Even if you resect the tumor with what you think are adequate margins, you are still likely going to be cutting through sarcoid tissue somewhere along the way. You are simply inoculating the whole area again, so the sarcoid is more likely to recur.
“Sarcoids are likely to recur, regardless of treatment selected. Probably the most effective treatment is surgical excision followed by some sort of chemotherapy, whether cisplatin, carboplatin injections or radiation. Most people inject the chemotherapy drug of choice with sesame oil, which increases the length of time the cisplatin or carboplatin stays in the surrounding tissue. Or you can make beads of chemo that you can implant, especially in areas that you can’t excise. These beads keep releasing the drug into the tissue, extending the length of effective treatment.
“There are several radiation treatments, including a linear accelerator and localized radiation beads called brachytherapy, but the newest way to increase the concentration of chemotherapy within the cells is electro-chemotherapy. This new method uses a machine that creates a current across the lesion which changes the polarity of the cell membrane and increases uptake of the drug. This form of treatment has actually shown the most promise. In one study, more than 90% of the treated horses had no recurrence in the several years following the treatment, and all of them remained free of sarcoid for greater than a year.
“The problem when you simply inject the drug without the added sesame oil, is that it just disperses very quickly into the body and doesn’t stay in the target area long enough. So, once you inject the area, you need to change the cells very quickly with current. The problem with this treatment is that the horse needs to be anesthetized. It’s not like an electrical jolt, but it does stimulate the muscles so you don’t want to do it with the horse standing. We are getting ready to buy one of these machines here, and more hospitals are offering this kind of treatment. This is a challenging disease, and the challenge grows exponentially with every failed treatment,” Smith concluded.